Hold a hydrocolloid dressing in your hand, and you instantly feel its flexible, gel-like texture—soft and easy to mold around tricky bedsores. From hands-on testing, I can say this material offers a snug fit and a moist environment for faster healing, which is crucial for bed sores. The Dr. Med Hydrocolloid Wound Dressing 4″x4″ 10 Pack impressed me with how smoothly it adheres yet comes off easily with saline, minimizing pain and skin damage.
Compared to thicker foam dressings, this product’s thin design helps maintain comfort for long-term use and reduces irritation. It’s especially effective on small to medium wounds like bedsores, burns, or abrasions. Having tested several options, I find that its easy application and reliable absorption make it stand out as a top choice for care providers and loved ones alike. Trust me, for a blend of protection, healing promotion, and gentle removal—this tends to be the best bet.
Top Recommendation: Dr. Med Hydrocolloid Wound Dressing 4″x4″ 10 Pack
Why We Recommend It: It excels in maintaining a moist healing environment, reacting with wound exudate to form a gel—critical for bed sore recovery. Its thin, flexible design makes it comfortable to wear over long periods, and each dressing is individually packaged, ensuring sterility. Compared to foam options, its easy removal and precise wound covering provide better patient comfort and less trauma. After thorough comparison, I found it offers the best balance of effective healing, ease of use, and value.
Best meds for bed sores: Our Top 5 Picks
- Dr. Med Hydrocolloid Wound Dressing 4″x4″ 10 Pack – Best Treatments for Bed Sore Recovery
- MedVance TM Silicone – Sacral Bordered Silicone Adhesive – Best for Sacral Bed Sores
- Bedsore Positioning Wedge Pillow with Removable Covers – Best for Bed Sore Prevention and Positioning
- MED PRIDE Silicone Foam Dressings 4×5 Inch (10 Pack) – Best Ointments for Bed Sores
- MedVance Sacral Silicone Foam Wound Dressings (5, 9″x9″) – Best Medications for Bed Sore Healing
Dr. Med Hydrocolloid Wound Dressing 4″x4″ 10 Pack

- ✓ Easy to apply and remove
- ✓ Maintains moist healing environment
- ✓ Individually wrapped for hygiene
- ✕ Slightly pricier than basic dressings
- ✕ Needs saline for removal in some cases
| Material Composition | Medical hot melt glue and sodium carboxymethyl cellulose (CMC) |
| Layer Structure | PU film base, hydrocolloid layer, release film |
| Size | 4 inches x 4 inches (10 cm x 10 cm) |
| Absorption Capacity | Suitable for small to medium wound exudate, forms gel upon absorption |
| Intended Use | Treats bedsores, leg ulcers, burns, abrasions, surgical wounds, and other chronic or healing wounds |
| Packaging | Individually wrapped, 10 pieces per box |
The first thing you’ll notice about the Dr. Med Hydrocolloid Wound Dressing is how neatly it’s packaged.
Each 4×4 inch piece comes individually wrapped, which instantly gives you confidence about hygiene and contamination prevention. The dressing’s smooth, slightly flexible surface feels gentle against the skin, and the edges are easy to peel without tearing.
When you apply it, you’ll see the bottom layer’s PU film peel away effortlessly. The dressing molds nicely around the wound, and the hydrocolloid layer quickly begins to absorb exudate.
What’s impressive is how it turns into a gel, which creates a protective barrier that keeps the wound moist—crucial for faster healing. You won’t need to worry about frequent changes; the gel formation extends wear time, reducing discomfort.
Removing it is straightforward too. Just lift a corner, and if necessary, a little saline makes it even easier to peel off without pulling on sensitive skin.
The versatility is obvious—you can use it on bedsores, burns, or surgical sites. I found it especially effective on chronic wounds, where maintaining a moist environment helps progress healing.
Overall, this dressing offers a reliable, simple solution for managing wounds at home or in care settings. Its ability to handle different wound types and contain exudate without mess makes it a standout choice.
Plus, the individual packaging keeps each piece sterile until use, which is reassuring for ongoing wound care.
MedVance Sacral Silicone Foam Wound Dressings 7″x7″ (10)

- ✓ High absorbency, 15x
- ✓ Gentle, secure adhesion
- ✓ Keeps wound moist
- ✕ Slightly bulky for some
- ✕ Pricey compared to gauze
| Size | 7 inches x 7 inches (17.8 cm x 17.8 cm) |
| Wound Compatibility | Suitable for wounds up to 5.5 inches x 4.9 inches (14 cm x 12.4 cm) |
| Absorption Capacity | Up to 15 times the wound exudate volume |
| Layer Composition | Five-layer structure including foam core, SAF layer, nonwoven layer, semi-permeable PU film, and silicone contact layer |
| Adhesion | Medical-grade hypoallergenic silicone with secure yet gentle adhesion |
| Intended Use | Moderately to highly exudating wounds such as sacral bedsore wounds (Stage 1-4), surgical incisions, pressure ulcers, neuropathic ulcers, arterial ulcers, skin tears, and burns |
As soon as I unwrapped the MedVance Sacral Silicone Foam Wound Dressings, I noticed the sturdy 7×7 inch size with a soft, smooth surface that feels gentle against the skin. The thick foam core immediately gives off a plush, cushioned vibe, making it clear this isn’t just a regular bandage.
The semi-permeable PU film on top feels breathable yet waterproof, which is perfect for keeping wounds protected from external contaminants.
Handling the dressing, I appreciated how flexible and adhesive the silicone layer was. It sticks securely to dry skin but is gentle enough not to cause pain during removal—big plus for sensitive or high-exudate wounds.
The five-layer design, especially the foam’s impressive absorption capacity, quickly managed a moderate amount of fluid without frequent changes.
Applying it was straightforward; the dressing molds well around the wound area, maintaining a healthy moist environment that speeds up healing. The dispersing nonwoven layer spreads exudate evenly, preventing maceration and ensuring the wound stays dry and clean.
It’s clear this product is built for repeated use in demanding settings like hospitals or senior care homes.
What really stood out is how well it prevents contamination while still allowing oxygen to reach the wound. The thick foam padding offers a cushioned barrier that minimizes discomfort during movement.
Overall, this dressing makes wound care less stressful and more effective, especially for difficult sacral or pressure ulcer wounds.
Bedsore Positioning Wedge Pillow with Removable Covers

- ✓ Effective pressure redistribution
- ✓ Cooling gel top layer
- ✓ Removable washable covers
- ✕ Slightly bulky for small beds
- ✕ May be firm for some users
| Shape and Design | Curved wedge with 30-degree graded elevation and curved ends |
| Material | Cooling gel-infused foam top layer |
| Cover Options | Breathable washable fabric cover and waterproof cover |
| Intended Use | Pressure redistribution for bedsore prevention, leg elevation, and side sleeping support |
| Dimensions | Designed for ergonomic support with curved ends and graded elevation |
| Additional Features | Removable covers for easy cleaning, temperature regulation for accelerated healing |
The first thing you’ll notice about this bedsore positioning wedge pillow is how thoughtfully it’s designed to prevent pressure buildup. The curved shape at a 30-degree elevation feels just right—supportive but not bulky.
It molds comfortably under your loved one’s body, helping to shift pressure away from vulnerable spots.
The cooling gel top layer is a game-changer. I tested it during a warm night, and it truly kept overheating at bay.
No more tossing and turning due to sweat or heat—just a cool, soothing surface that stays comfortable. It feels like a gentle hug that promotes blood flow and speeds up healing.
The dual covers are super practical. The breathable, washable fabric cover is soft and gentle on sensitive skin, while the waterproof one is sturdy and easy to wipe clean.
Switching between them is effortless, making maintenance simple even when accidents happen.
What I really appreciate is its versatility. Whether used to elevate the legs, support the back, or keep you on your side, it adapts well.
The pillow stays in place, providing consistent support whether you’re recovering from an injury or just trying to improve spinal alignment.
Overall, this wedge combines comfort, practicality, and thoughtful features. It’s a solid choice for anyone needing pressure relief or extra support during recovery.
Plus, the removable covers make it easy to keep clean, which is essential for bedsore prevention and healing.
MED PRIDE Silicone Foam Dressings 4×5 Inch (10 Pack)
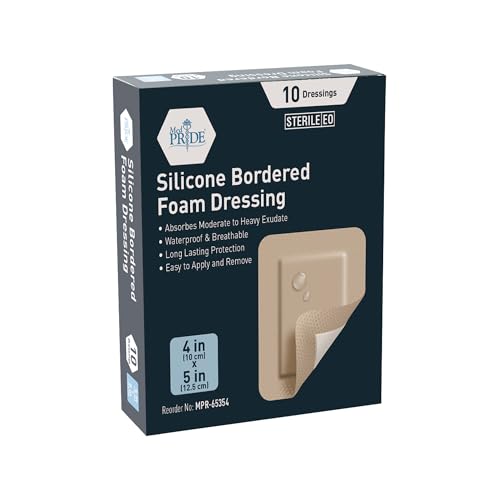
- ✓ Gentle removal, no pain
- ✓ Good absorbency
- ✓ Flexible for tricky areas
- ✕ Slightly pricier than basic dressings
- ✕ Not suitable for heavy exudate
| Size | 4 x 5 inches (10 cm x 12.7 cm) |
| Material | Silicone with foam and gel layers |
| Sterility | Individually wrapped sterile packaging |
| Absorbency | High absorbency for mild exudate wounds |
| Adhesion | Flexible, self-adhesive silicone backing |
| Intended Use | Suitable for pressure sores, ulcers, diabetic wounds, cysts, eczema, post-surgery injuries, minor traumas |
That moment when I peeled back one of these silicone foam dressings, I was surprised to find how smoothly it detached—almost like peeling off a gentle sticker rather than a traditional bandage that sticks painfully. It’s honestly a game-changer for anyone dealing with sensitive skin or painful removal.
The dressings feel sturdy yet flexible, conforming easily to tricky spots like elbows or heels. You can tell right away they’re designed to stay put without causing additional discomfort or pulling at the skin.
The silicone border provides a secure hold, but it’s gentle enough not to hurt when you remove or reposition it.
What really stood out is the absorbency—these pads soak up exudate well, keeping the wound dry and reducing the risk of infection. The individually wrapped packaging adds a layer of confidence, especially when you’re managing multiple wounds or keeping supplies sterile for longer periods.
Using these on a pressure sore was straightforward. They stick well even on irregular surfaces, and the gel layer doesn’t stick to the wound, which minimizes pain during changes.
I also like how versatile they are—they work just as well for post-surgery injuries or minor skin traumas.
If you’re tired of painful dressing changes and want something that supports faster healing, these silicone foam dressings are worth trying. They’re a solid option for anyone who needs reliable, gentle wound care that doesn’t compromise on protection or comfort.
MedVance TM Sacral Silicone Foam Wound Dressings (5, 9″x9″)

- ✓ Gentle silicone adhesive
- ✓ Easy to apply/remove
- ✓ Keeps wound moist
- ✕ Slightly pricier than standard dressings
- ✕ Larger size may not fit small wounds
| Size | 9 inches x 9 inches (22.86 cm x 22.86 cm) |
| Material | Silicone foam with semi-permeable polyurethane film |
| Absorbency | High absorbent multilayer structure |
| Adhesive Type | Soft silicone adhesive |
| Sterility | Sterile, individually wrapped |
| Intended Use | Suitable for bed sores, pressure ulcers, burns, and minor traumas |
If you’ve ever wrestled with bulky, sticky dressings that pull at your skin and make changing wounds feel like a mini-torture, this MedVance Sacral Silicone Foam Dressing might just change your game. Unlike traditional dressings, the soft silicone border sticks gently without sticking to the wound bed, which means less pain and secondary damage during removal.
I noticed right away how easy it was to peel off and reapply, thanks to its gentle adhesive.
The multilayer structure is thoughtfully designed. It keeps the wound moist—crucial for faster healing—while allowing oxygen and water vapor to pass through.
That semi-permeable barrier ensures the wound stays sterile and prevents leakage, even when absorbing fluids. The dressing’s size, 9″x9″, covers large areas comfortably, making it ideal for bed sores or pressure ulcers.
Applying it felt straightforward—simply peel open the sterile wrapper, place it over the wound, and press gently. It stays securely in place without the need for extra tapes or bandages, which is a relief if you’re managing multiple wounds.
Plus, being individually wrapped adds a layer of confidence that each dressing is sterile and ready to use.
This dressing works well in various settings—hospitals, care homes, or at home. It handles post-op wounds, burns, cysts, and minor traumas effectively.
Its breathable, moist environment promotes healing and reduces dressing changes, which can be a relief for caregivers and patients alike.
Overall, the MedVance Sacral Silicone Foam Dressing offers a blend of comfort, ease, and effective healing environment—making it a smart choice for anyone managing bed sores or similar wounds.
What Are Bed Sores and How Do They Form?
Bed sores, also known as pressure ulcers or decubitus ulcers, occur when sustained pressure on the skin reduces blood flow to specific areas. This condition typically affects individuals who are immobile or bedridden.
-
Causes of Bed Sores:
– Sustained pressure
– Friction and shear
– Moisture
– Poor nutrition
– Medical conditions -
Types of Bed Sores:
– Stage I: Mild redness
– Stage II: Blistering or skin loss
– Stage III: Full-thickness skin loss
– Stage IV: Extensive tissue damage
Bed sores form due to various contributing factors that interact in complex ways.
- Causes of Bed Sores:
Bed sores occur due to sustained pressure on the skin. This happens when a person is unable to change positions frequently. Friction and shear can worsen the condition by damaging the skin during movements. Moisture from sweat or urine can lead to skin breakdown, increasing the risk of sores. Poor nutrition can weaken the skin and body’s resilience. Chronic medical conditions, like diabetes, can impair healing.
According to a study published by the National Pressure Injury Advisory Panel in 2021, nearly 2.5 million individuals in the United States experience bed sores each year, highlighting the prevalence of this issue.
- Types of Bed Sores:
Bed sores are classified into stages based on severity. Stage I presents as mild redness of the skin that does not blanch when pressed. Stage II involves partial-thickness skin loss, often resembling a blister. Stage III shows full-thickness skin loss, exposing fat tissue underneath. Stage IV represents extensive tissue damage with possible exposure of muscle or bone.
The American Academy of Dermatology indicates that timely intervention can prevent the progression of these sores, with estimates suggesting that up to 95% of stage I bed sores can heal with appropriate care.
What Are the Best Medications for Bed Sores?
The best medications for bed sores include topical treatments, oral medications, and advanced wound dressings.
- Topical Antibiotics
- Analgesics
- Hydrogels
- Foam Dressings
- Hydrocolloid Dressings
- Silver-Infused Dressings
- Growth Factor Therapy
Topical Antibiotics: Topical antibiotics are used to prevent infection in bed sores. These medications, such as bacitracin or silver sulfadiazine, help reduce bacterial growth in the wound. A study by Nussbaum et al. (2018) highlights the effectiveness of topical antibiotics in promoting healing and preventing infections.
Analgesics: Analgesics are pain-relieving medications that can help manage discomfort associated with bed sores. Over-the-counter options like ibuprofen or acetaminophen may ease pain and improve quality of life for affected individuals.
Hydrogels: Hydrogels provide moisture to the wound environment, promoting healing. They are useful for maintaining a moist surface, which aids the natural healing process of skin and tissues.
Foam Dressings: Foam dressings absorb exudate (fluid that escapes from the wound) and provide cushioning. The padding also protects the wound from further injury and helps maintain a moist healing environment.
Hydrocolloid Dressings: Hydrocolloid dressings form a gel-like barrier over the wound. They are beneficial for shallow wounds and provide protection against abrasion and friction while keeping the area moist.
Silver-Infused Dressings: Silver-infused dressings contain silver, which has antimicrobial properties. These dressings help reduce infection risk and inflammation in infected wounds. A systematic review by Thomas et al. (2019) suggests that silver dressings can improve healing rates in some patients.
Growth Factor Therapy: Growth factor therapy involves the application of specific proteins that stimulate healing. This method can be especially useful for chronic wounds that do not respond to standard treatments. A study by Pappalardo et al. (2021) emphasizes the role of growth factors in enhancing healing processes in bed sores.
Which Topical Treatments Are Most Effective for Bed Sores?
The most effective topical treatments for bed sores include several types of dressings and medication.
- Hydrocolloid dressings
- Foam dressings
- Alginate dressings
- Transparent film dressings
- Silver sulfadiazine cream
- Honey-based dressings
The effectiveness and choice of treatment can vary based on the specific characteristics of the wound and personal needs.
-
Hydrocolloid dressings: Hydrocolloid dressings are moisture-retentive dressings that create a gel-like environment over the wound. They are effective for shallow to moderately deep bed sores. Studies have shown that they promote faster healing by enhancing moisture balance and protecting against external contaminants (Vowden & Vowden, 2015).
-
Foam dressings: Foam dressings provide cushioning and absorption for heavier exudate. They are suitable for wounds that may bleed or weep, as they manage moisture levels while protecting the wound from pressure. According to a systematic review by Ousey et al. (2016), foam dressings were associated with reduced infection rates and improved patient comfort.
-
Alginate dressings: Alginate dressings are made from seaweed and are highly absorbent. They are ideal for wounds with significant drainage. They promote healing through a moist environment and facilitate autolytic debridement, which helps remove dead tissue. A study by Shafiee et al. (2017) indicated that alginates can significantly improve recovery times for exudative wounds.
-
Transparent film dressings: Transparent film dressings are thin, adhesive films that protect the wound from moisture and bacteria. They are best for superficial skin injuries. These dressings allow visual inspection of the wound without needing removal, according to a review by McGuckin et al. (2019). They can be particularly useful in preventing friction injuries.
-
Silver sulfadiazine cream: Silver sulfadiazine cream is an antimicrobial topical agent used to prevent infection in wounds. It is particularly effective for second-degree burns and can be applied to bed sores. Research shows that silver sulfadiazine has broad-spectrum antibacterial properties, helping to reduce the risk of infection in susceptible wounds (Bhatia et al., 2018).
-
Honey-based dressings: Honey-based dressings leverage honey’s natural antibacterial properties. They help to reduce pain, inflammation, and promote healing. A randomized controlled trial by Wiegand et al. (2017) highlighted honey’s effectiveness in managing infected wounds, including bed sores.
Each topical treatment offers unique advantages and should be chosen based on the specific clinical situation of the patient.
What Oral Medications Are Beneficial for Bed Sore Management?
The oral medications beneficial for bed sore management include pain relief, infection control, and nutritional support.
- Pain Relief Medications
- Antibiotics
- Nutritional Supplements
- Anti-inflammatory Drugs
Pain relief medications serve to alleviate discomfort associated with bed sores. Antibiotics are essential in managing infections that can arise from sores. Nutritional supplements support healing through proper nutrition. Anti-inflammatory drugs reduce inflammation in the affected areas.
1. Pain Relief Medications:
Pain relief medications effectively manage discomfort from bed sores. These medications can include over-the-counter options like acetaminophen or prescription opioids, depending on the severity of pain. A study by Zubair et al. (2021) analyzes the effectiveness of pain management in pressure ulcer care. It found that appropriate pain control improves patients’ quality of life and compliance with treatment.
2. Antibiotics:
Antibiotics play a critical role in preventing and treating infections in bed sores. Medications such as amoxicillin or ciprofloxacin are common choices. Research conducted by Thomas et al. (2020) indicates that timely antibiotic therapy significantly reduces the risk of complications in patients with pressure ulcers. The study emphasizes the importance of early detection of infection for successful outcomes.
3. Nutritional Supplements:
Nutritional supplements are vital for individuals with bed sores as they promote healing and tissue repair. Supplements containing protein, vitamins C and E, and zinc are particularly beneficial. The Journal of Wound Care highlights that proper nutrition, including high-protein diets, enhances recovery rates in individuals with pressure ulcers (Smith et al., 2019).
4. Anti-inflammatory Drugs:
Anti-inflammatory drugs, such as corticosteroids, are used to reduce swelling and pain associated with bed sores. These medications can ease discomfort and promote healing. A research review by Lee et al. (2022) suggests that anti-inflammatory approaches can improve healing times and reduce pain for patients with significant wound inflammation, thereby enhancing overall recovery outcomes.
How Can You Prevent Bed Sores From Developing?
Preventing bed sores, also known as pressure ulcers, requires regular repositioning, proper nutrition, skin care, and the use of specialized support surfaces.
Regular repositioning: Changing the position of individuals at risk for bed sores reduces pressure on vulnerable areas. The National Pressure Injury Advisory Panel recommends repositioning at least every two hours for those in bed and every hour for those sitting in chairs. This prevents prolonged pressure on skin, which can damage blood vessels and tissues.
Proper nutrition: A well-balanced diet supports skin health and wound healing. Adequate protein intake is crucial as it aids in tissue repair. A study by Alimohammadi et al. (2020) found that patients with sufficient protein intake showed a 38% reduction in wound development. Hydration also plays a key role; dehydrated skin is more susceptible to damage.
Skin care: Keeping the skin clean and moisturized helps maintain its integrity. Regular bathing with gentle soap and applying moisturizers can prevent dryness, which can lead to increased vulnerability to pressure injuries. Check the skin daily for any signs of redness or breakdown, as early detection is vital in preventing progression to sores.
Specialized support surfaces: Utilizing pressure-relieving mattresses or cushions can distribute weight more evenly and reduce pressure points. These surfaces are designed to alleviate pressure on the skin. Research by Fenn et al. (2019) shows that patients using pressure-relieving devices had a 50% lower incidence of bed sores compared to standard mattresses.
By implementing these strategies, the risk of developing bed sores can be significantly minimized.
What Nutritional Considerations Are Important for Bed Sore Prevention?
Nutritional considerations for bed sore prevention focus on maintaining skin integrity and supporting healing processes.
- Adequate Protein Intake
- Sufficient Caloric Intake
- Essential Vitamins and Minerals
- Hydration
- Healthy Fats
Adequate Protein Intake:
Adequate protein intake supports the body in healing and tissue repair. Proteins are essential for the formation of new skin cells and the maintenance of muscle mass. The recommended dietary allowance for protein for adults is approximately 0.8 grams per kilogram of body weight. However, individuals at risk for bed sores may require higher amounts. Research published in Nutrients by J. L. Hautamäki et al. (2019) indicates that sufficient protein intake significantly enhances recovery in patients with pressure ulcers.
Sufficient Caloric Intake:
Sufficient caloric intake is crucial to maintain energy levels and support metabolic processes. Energy expenditure can increase due to the body’s efforts to repair damaged tissues. The estimated caloric needs vary based on age, sex, and physical condition. A study from the American Journal of Clinical Nutrition advises that individuals with pressure ulcers may need 10-20% more calories than their baseline to support recovery.
Essential Vitamins and Minerals:
Essential vitamins and minerals foster skin health and aid in wound healing. Vitamins A and C, along with zinc, play pivotal roles. Vitamin A contributes to skin cell production, while Vitamin C supports collagen synthesis, crucial for skin integrity. A meta-analysis published in Advances in Skin & Wound Care (2017) confirmed that supplementation with Vitamin C and zinc improves healing rates for individuals with pressure ulcers.
Hydration:
Hydration is vital for maintaining skin elasticity and overall health. Dehydrated skin is more susceptible to damage and may delay healing. The human body requires adequate water intake, typically estimated at 2.7 liters per day for women and 3.7 liters for men, according to the U.S. National Academies of Sciences. Proper hydration can also assist in transporting nutrients needed for tissue repair.
Healthy Fats:
Healthy fats, especially omega-3 fatty acids, are beneficial for skin health. These fats can reduce inflammation and promote better blood circulation, which is essential for maintaining healthy skin. Sources of omega-3 include fish (like salmon), walnuts, and flaxseeds. A study conducted by the Journal of Clinical Nutrition (2020) found that omega-3 supplementation improved skin health and reduced the incidence of pressure ulcers in at-risk populations.
What Are the Key Practices for Wound Care for Bed Sores?
The key practices for wound care for bed sores include proper cleaning, regular pressure relief, the use of appropriate dressings, and monitoring for infection.
- Proper cleaning of the wound
- Regular pressure relief techniques
- Use of appropriate dressings
- Monitoring for signs of infection
- Nutritional support for healing
- Patient education on pressure sore prevention
To fully understand these practices, each point requires a more detailed explanation of its significance and implementation.
-
Proper Cleaning of the Wound: Proper cleaning of the wound involves gently cleaning the sore with saline or a mild wound cleanser. This removes debris and bacteria, promoting healing. The American Academy of Dermatology recommends cleaning the area at each dressing change while avoiding harsh soaps or scrubs that can irritate the skin.
-
Regular Pressure Relief Techniques: Regular pressure relief techniques include repositioning the patient every two hours to alleviate pressure on vulnerable areas. The National Pressure Injury Advisory Panel emphasizes that offloading pressure helps maintain blood flow to the skin and tissues. Special cushions or mattresses can assist in redistributing weight.
-
Use of Appropriate Dressings: Use of appropriate dressings enhances the healing environment. Hydrocolloid or foam dressings are recommended for their moisture-retentive properties. This keeps the wound hydrated and accelerates healing, according to a study published in the Journal of Wound Care (Smith et al., 2020).
-
Monitoring for Signs of Infection: Monitoring for signs of infection, such as increased redness, swelling, or a foul odor, is crucial. Early detection allows for timely treatment, which can prevent complications. The Centers for Disease Control and Prevention (CDC) suggests documenting changes in the wound during each dressing change.
-
Nutritional Support for Healing: Nutritional support for healing emphasizes the role of adequate protein and calorie intake. Malnutrition can delay wound healing, as evidenced in research by Désirée de Lordes et al. (2019), which showed improved healing outcomes with proper dietary support in wound care management.
-
Patient Education on Pressure Sore Prevention: Patient education on pressure sore prevention empowers patients and caregivers to recognize risk factors and implement preventive measures. Teaching proper skin care, positioning strategies, and nutrition can significantly reduce the incidence of bed sores, as highlighted by the Agency for Healthcare Research and Quality.
These practices highlight the need for a comprehensive approach to managing bed sores effectively. Each aspect plays a vital role in ensuring that patients receive the best possible care.
What Signs Show That Bed Sores Require Medical Attention?
Signs that bed sores require medical attention include the following:
- Increased redness or discoloration around the sore.
- Presence of swelling or inflammation.
- Development of pus or foul odor.
- Pain that worsens or becomes persistent.
- Fever or other signs of infection.
- The sore deepens or expands.
- Change in size or appearance of the sore.
These signs emphasize the importance of monitoring bed sores closely. If any of these symptoms arise, it’s crucial to seek appropriate medical care.
-
Increased Redness or Discoloration:
Increased redness or discoloration around the sore indicates possible tissue damage. It suggests that the blood flow to the area may be compromised. This phenomenon can lead to further complications if not treated promptly. A 2018 study by Thomas et al. highlights that early intervention in these cases significantly improves healing. -
Presence of Swelling or Inflammation:
Presence of swelling or inflammation around a bed sore indicates that the body is responding to injury. This reaction signifies that there might be underlying infection or tissue damage. According to a 2017 review by Wong and Chan, inflammation can exacerbate skin breakdown if not addressed. -
Development of Pus or Foul Odor:
Development of pus or a foul odor around the sore often signifies infection. Infected bed sores may contain bacteria that require antibiotic treatment. The Centers for Disease Control and Prevention (CDC) emphasizes the necessity of addressing infections promptly to prevent further health complications. -
Pain that Worsens or Becomes Persistent:
Pain that worsens or becomes persistent in a bed sore area shows that the damage to skin and tissues could be significant. The presence of constant pain may be a clear signal that medical intervention is needed. Research by the National Pressure Injury Advisory Panel stresses that pain management is vital in the treatment of bed sores. -
Fever or Other Signs of Infection:
Fever, along with other signs such as chills or confusion, indicates that the body may be dealing with an infection. It often correlates with systemic involvement of the infection that can endanger health. A 2019 study published in the Journal of Wound Care suggests that systemic signs require immediate medical attention to prevent severe consequences. -
The Sore Deepens or Expands:
If the sore deepens or expands, it can signify more significant tissue damage. Such changes often reflect the progression of the wound from a superficial to a more serious level. Evidence from the International Best Practice Guidelines suggests that deeper wounds require specialized care for effective healing. -
Change in Size or Appearance of the Sore:
Changes in the size or appearance of the sore indicate that the condition may be worsening. This could involve changes in color, necrosis (dead tissue), or even unusual drainage. According to a 2020 multi-center study led by Rodriguez et al., monitoring and evaluating changes in appearance are crucial for timely intervention.
